“There are many sources of water coming into the Salinas Valley watershed, and I guarantee you they all have generic E. coli.”
– Christopher Rose, California’s Central Coast Regional Water Quality Control Board


“Currently we are advising consumers not to eat any fresh spinach
or salad blends containing spinach grown in three counties in California
implicated in the current E. coli O157:H7 outbreak: Monterey County, San Benito County and Santa Clara County. Fresh spinach grown outside these counties can be safely eaten. Frozen and canned spinach have not been identified as part of the outbreak and can be safely eaten even if grown in Monterey, San Benito and Santa Clara Counties in California.”
– CDC Advisory, Sept. 23, 2006
September 23, 2006 Davis, California – By Friday, September 22, 2006, 157 Americans in 23 states had become ill from a nationwide E. coli O157:H7 contamination of spinach. Eighty-three people had been hospitalized; twenty-seven had developed a type of kidney failure called hemolytic-uremia, and one had died.
E. coli O157:H7 can live in the intestines of cattle and other animals without making the animals sick. The bacteria is then shed in feces. This particularly dangerous E. coli bacteria can be found in undercooked meats and raw spinach, sprouts, lettuce, unpasteurized milk and juice.
According to the Centers for Disease Control and Prevention (CDC), the primary symptom of E. coli O157:H7 in humans is blood red stools or diarrhea. Each year on average, about 73,000 cases of this specific E. coli infection in humans are reported to health authorities, including 61 deaths.
Children can be especially vulnerable and the CDC is also investigating the death of a 2-year-old girl who died September 20, after being fed spinach liquefied in a blender.
By then, an opened bag of fresh spinach was found in the refrigerator of an Albuquerque, New Mexico, resident who became ill with bloody dysentery. That “confirmed positive sample” was in a bag of Dole baby spinach with a “best if used by Aug. 30” date. The source of the spinach was Natural Selection Foods, the California food producer that is now the focus of the E-coli investigation.
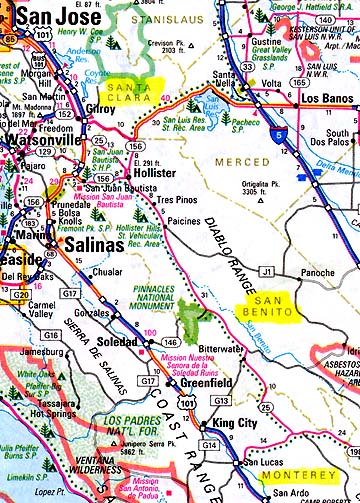
That bag lead FDA investigators to the Salinas Valley in California, where almost 75 percent of U. S. spinach crop is grown. That search narrowed the E. coli-contaminated spinach down to three counties: Monterey County, San Benito County and Santa Clara County.
The Los Angeles Times reported on September 21, 2006: “Many creeks and streams near the region’s spinach fields are known to contain 12,000 or more E. coli organisms per 100 milliliters of water — thirty times the Environmental Protection Agency’s standard. California officials are currently studying ways to bring the Salinas River watershed into compliance with the EPA’s rules. Christopher Rose of the California’s Central Coast Regional Water Quality Control Board said: ‘There are many sources of water coming into the Salinas Valley watershed, and I guarantee you they all have generic E. coli.”
In the Salinas Valley, 97% of irrigation water is pumped up from private wells. The Sacramento Mercury News reported there is no law for mandatory inspection of well water. The newspaper also learned that the federal government’s Occupational Safety and Health Administration (OSHA) inspects only about a thousand California crop fields a year; the state has several thousand farms.
In November 2005, the U. S. Food and Drug Administration investigated a previous outbreak of E. coli in Salinas Valley spinach. FDA’s Chief Medical Officer for Food Safety and Applied Nutrition told a press conference on September 20, “More should have been done (then). We are learning from this (new) outbreak.” Oddly, in eighteen E.coli contaminations since 1995, the FDA has never identified a specific farm or source of the dangerous bacteria.
The National Institutes of Health reported this week that “92 percent (E.coli victims) were sickened between August 19 and September 5. The earliest onset of illness known to be linked to spinach consumption was on August 19. All told, 113 of the victims were females, and 11 were children under 5.
“On Wednesday (September 20), Arizona and Colorado became the latest states to report their first confirmed cases of E. coli. Also reporting cases have been California, Connecticut, Idaho, Illinois, Indiana, Kentucky, Maine, Michigan, Minnesota, Nevada, Nebraska, New Mexico, New York, Ohio, Oregon, Pennsylvania, Utah, Virginia, Washington, Wisconsin and Wyoming. Wisconsin has the largest number of reported cases, 40. The next largest number of cases are in Utah, which has 17, followed by Ohio with 20, according to the CDC.
“Consumers should continue to throw away any fresh packaged spinach they may have bought in the past few weeks and not buy more until the public health warning is lifted. Washing spinach won’t help because the bacteria is too tightly attached.”
What does “too tightly attached” mean exactly? I asked Dean Cliver, Ph.D., Professor of Food Safety in the School of Veterinarian Medicine at the University of California-Davis. Prof. Cliver received his Ph. D. from Ohio State University in Dairy Science in 1960. For the next thirty-five years, he worked for the Food Research Institute at the University of Chicago and University of Wisconsin-Madison. He has been at the University of California in Davis since 1995.
Interview:
Dean Cliver, Ph.D., Prof. of Food Safety, School of Veterinarian Medicine, University of California-Davis : “The name, E. coli O157: H7 tells us two things: this particular bacteria has a 157 “O” antigen and a number 7 “H” antigen. It’s the same bad guy that caused the Jack In The Box outbreak that got over 700 people. [ In 1993, hundreds of people were injured and four children died after eating at Jack in the Box restaurants. The primary cause of the outbreak was E. coli-contaminated hamburger patties manufactured and sold to the restaurant chain by one of its suppliers. If undercooked, those hamburgers made people sick.]
It’s the same bacteria that caused the Odwalla outbreak and 70 some illnesses. [ California-based Odwalla Inc., the maker of Odwalla fruit juices, issued a nationwide recall on November 1, 1996, of all its products containing apple juice after health officials linked it to an outbreak of E. coli O157:H7 bacterial poisoning.]
One was under-cooked hamburgers; the other was raw apple juice cider. There have been other outbreaks recently, including some with baby lettuce and baby spinach.
Why Can’t the E. coli Bacteria Be Washed Off Contaminated Plants?
As far as how E. coli gets into the plants – this has not been well studied. There are people who are saying it comes up through the roots from irrigation water. I think irrigation water is a prime suspect, but I don’t think the root transport is too likely. It seems to me that when leaves get wet, a certain amount of whatever is on the surface goes in through the little pores that lets the air diffuse in and out of the leaves.
So, there is a spongy layer inside the leaf that I suspect is where the E. coli O157:H7 hangs out. Because it’s not just out there on the surface of the leaves, you can’t wash it off.
DOES ANYONE KNOW WHAT TEMPERATURE THIS PARTICULAR E. COLI BACTERIA CAN STAND WITHOUT DYING?
E. coli is not an especially heat resistant bacteria, so you would have a hard time finding any of them still alive in frozen spinach after the hot blanching before freezing. And if you cook your spinach is going to take care of it.
IS THERE A TEMPERATURE AT WHICH THIS BACTERIA WILL DIE?
You can look at what the FDA said with the hamburger cases. They said that you ought to cook hamburger to 155 to 160 degrees F. for several minutes. They say if you grill burgers, you should get a thermometer and make sure the inside temperature of the burger is at least 155 to 160 degrees. There’s no secret about killing E. coli O157:H7.
BUT THE TEMPERATURE HAS TO BE AT LEAST 155 DEGREES F. FOR A COUPLE OF MINUTES?
Yes, or up to 160 degrees F.
WHAT HAPPENS TO SPINACH AT THAT TEMPERATURE FOR TWO MINUTES?
When I mentioned blanching to freeze spinach, people who grow their own spinach and freeze it, probably blanch above that temperature. So it’s going to wilt, but it’s not necessarily going to go all mushy. But if you put it in a pot and boil it the way some people boil greens traditionally, eventually it will get mushy – but then it’s very safe to eat. [ Editor’s Note: Italians have a long tradition of cooking spinach with garlic that’s very safe. See More Information below.]
HOW LONG WOULD A PERSON HAVE TO BOIL GREENS TO MAKE SURE THERE WAS NO E. COLI BACTERIA?
If you bring it to a boil, it’s gone. Boiling is 212 degrees F., so from a safety standpoint, just getting the leaves themselves to the temperature of boiling water kills the bacteria.
What Is Source of This E. coli O157:H7 Outbreak? Could it be contaminated well water?
This is not the first outbreak. I know of at least one other from the Salinas Valley recently and probably four or five outbreaks from leaf lettuce. There have been a lot of investigations done, but so far they have not found what I call a ‘smoking gun.’ The FDA does not know how the contamination takes place. I know FDA is back in all over the place in the Salinas Valley sampling fields. My thought is that they need to cast a broader net than they have before.
Most of the growers grow things that are going to be eaten raw like baby spinach and leaf lettuce and they are using well water. To the best of their knowledge, the water is safe for plant irrigation, but nobody says it is safe to drink.
We don’t even know how the water gets down there to the aquifer that the well is pulling it from. So my feeling is that we need to do some ground water mapping and find out what the sources are for the water that comes out of those wells used for irrigation. We might be able to trace it back to some cattle somewhere.
There are no cattle in sight of those Salinas Valley fields. But once in awhile, stuff runs off dairy farms into streams, so I think most growers are pretty shy about using surface water for irrigation. I think they tend to want to have a well.
YOU ARE MENTIONING CATTLE BECAUSE E.COLI BACTERIA COULD ONLY COME FROM THE FECES OF ANIMALS?
From animals and it can be transmitted from person-to-person. We’ve had outbreaks in daycare centers that show people produce it, too. But people get sick mostly when they are infected with E.coli O157:H7 and cattle don’t. So the better generic term is ‘ruminants’ – cattle, goats, sheep and even deer and elk – can be reservoirs, can carry E.coli O157: H7 without getting ill.
When you look at the quantity of manure that is produced in the U. S., cattle have got all the others beat. So, the perception is that if E.coli O157:H7 turns up in a waterway, you go back up stream and look for cattle.
BOTTOM LINE, YOU’RE SAYING THERE IS NO CLEAR UNDERSTANDING OF HOW THIS PARTICULAR E.COLI BACTERIA GETS INTO PLANTS SUCH AS SPINACH?
That is as best I can tell a fact. FDA has been to the fields and farms in the Salinas Valley, California, repeatedly and told them: ‘You’ve got to be careful!’ But I don’t find their recommendations specific. If they knew exactly what had caused these earlier outbreaks, then maybe we would be on a track different than we have now. But as far as how the bacteria got into the spinach in this instance, I think FDA is basically clueless. Hopefully the field investigation they are doing there will turn up something, but they’ve done field investigations before.
Why Is the E. coli O157:H57 So Dangerous to Humans?
Apparently Mother Nature did some cross-breeding. We have a genus of bacteria that has caused devastating disease in humans for centuries called Shigella, a gastrointestinal bacteria that causes dysentery. The genes that seem to be in the E. coli that make people so sick are genes that it shares with the Shigella bacteria. But Shigella only infects people, not animals. So, somehow or other, these two bacteria got together. Some of the genes that make Shigella so dangerous to humans got into that E. coli O157:H7. But they don’t hurt cattle, so they can hang out in the intestines of a cow for periods of time and are shed through feces.
What Are Human Symptoms of E. coli O157:H7 Infection?
The most characteristic symptom of this E. coli is bright red blood in the stool. That can happen to anyone who gets infected. Kids under 5-years-old are especially susceptible to kidney failure – something called hemolytic-uremia syndrome.
Older people above 65 are subject to a kind of kidney failure that causes blood clotting problems as well. That’s called thrombotic thrombocytic purpura. You wind up with hemorrhages under the skin.
So, O157:H7 and Shigella bacteria infections are more life threatening. Kids who get hemolytic-uremia syndrome might lose their kidneys.
Do Antibiotics Help?
Antibiotics don’t do any good. In most instances, that is not considered appropriate. People who take antibiotics for this particular E. coli are probably worse off – not because the bacteria is resistant to the antibiotics, but because the Shiga toxins it produces are liberated more quickly, and your body might get more of a shock, as a result of the antibiotic attacking the bacteria – than if you just let your body cope with the bacteria as best it can.
[ Editor’s Note: Wikepedia says Shiga toxins are named for Kiyoshi Shiga, who first described the bacterial origin of dysentery caused by Shigella dysenteriae. It’s a family of related toxins with two major groups, Stx1 and Stx2, whose genes are considered to be part of the genome of lambdoid prophages. The most common sources for Shiga toxin are the bacteria Shigella dysenteriae and the Shigatoxigenic group of Escherichia coli (STEC), which includes serotype O157:H7 and other enterohemorrhagic E. coli. ]
The majority of people do get over it and hopefully don’t have long-term ill effects. But if the kidneys are involved, it can lead to kidney transplant.
IS THERE ANY EFFECTIVE TREATMENT?
As far as I know, it’s all what is called ‘supportive’ – trying to keep patients hydrated. If your kidneys decide to shut down, then you might be put on dialysis until they can replace a kidney. Really there is no way to make the E. coli infection go away quickly.”
More Information:
On Sep 23, 2006, at 10:17 AM, [email protected] wrote:
“Linda,
I listened with great interest to your show on Coast last night. Your report on the spinach contamination was excellent. While listening I remembered what my Italian Grandmother use to do with spinach. She use to cook it and then drain all the water out. While that was going on, she would take some extra virgin olive oil and brown some fresh garlic in it. Then she would add the drained spinach for just a few minutes and serve it with a little salt. We never got sick.
My Grandmother also would do this with other leafy veggies as well, such as mustard greens, Swiss chard, endives etc.
Linda, thank you so much for the important work you do, I always learn much more from you than I do listening to the so-called ‘main stream’ media!
Thank you so much,
Joe Who
www.joewho.com“
For further information about environmental contaminations, please see reports below in the Earthfiles Archives.
- 06/23/2006 — Morgellons Agony of Skin Lesions and “Brain Fog”
- 03/21/2006 — One Way H5N1 Bird Flu Could Adapt to Humans
- 08/26/2005 — What Is Killing Amphibians Around the World?
- 06/27/2005 — Second American Mad Cow Case – Texas Herd Source?
- 06/21/2005 — CDC Reports First 2005 Human Case of West Nile Virus in Kansas
- 06/03/2005 — West Nile and Bird Flu: Two Increasingly Dangerous Viruses
- 04/07/2005 — Chronic Wasting Disease Has Spread to New York State Captive Deer
- 03/12/2005 — Could Avian Flu H5N1 Cause the Next Pandemic?
- 02/26/2005 — Collapse of Societies: From Easter Island to Iraq – to Western World?
- 08/01/2004 — Sixth Straight Year Hundreds of Birds Die at Roestler Lake, North Dakota.
- 03/12/2004 — Milkweed Poisoning Killed the 31 Cedaredge, Colorado Cattle
- 02/20/2004 — New Form of Mad Cow Disease Resembles Human Creuzfeldt-Jakob Disease (CJD)
- 01/27/2004 — FDA Outlaws Cattle Blood in Livestock Feed
- 12/16/2003 — Colorado Doctor Suspects Fujian Flu Has Hit Elderly Hard
- 04/26/2003 — Beijing Quarantines 4000 Residents Exposed to SARS; Third Hospital Sealed Off
- 04/25/2003 — Coronavirus Expert Questions Animal Source for SARS
- 04/18/2003 — SARS Coronavirus Can Spread in Urine and Feces
- 4/16/2003 — New Coronavirus Causes SARS Symptoms in Monkeys
- 04/03/2003 — SARS Current World Total: 2285 Cases and 79 Deaths; First Brazil Case Brings SARS Spread to 4 Continents
- 04/02/2003 — SARS Pneumonia Cases Increasing in U. S. and Worldwide
- 03/31/2003 — Hong Kong Enforces Quarantine in Amoy Garden Apartments to Slow SARS Pneumonia Spread
- 03/30/2003 — SARS Pneumonia Closes Second Toronto Hospital; Doctor Who First Recognized SARS Has Died of SARS
- 03/29/2003 — SARS Pneumonia Spreads Despite Quarantines; American Patient’s Sister Describes Agony
- 03/28/2003 — Current SARS Information from W. H. O. and CDC
- 03/24/2003 — SARS Pneumonia Cases Are Increasing and Singapore Orders Quarantines
- 03/22/2003 — Medical Experts Are Worried About the New SARS Pneumonia
- 03/18/2003 — SARS Pneumonia Tentatively Identified as Paramyxoviridae Virus
- 01/18/2003 — Can the United States Cope with Bioterrorism Attacks?
- 09/28/2002 — 2002 Mad Cow Disease and West Nile Fever Updates
- 07/20/2002 — Extinctions of Earth Life Are Accelerating Rapidly
- 04/06/2002 — Chronic Wasting Disease Spreads to Wisconsin White-Tailed Deer
- 10/10/2001 — Three Anthrax Inhalation Cases In Florida FBI Opens Criminal Probe – Nano Bomb Update
- 04/24/2001 — Chronic Wasting Disease (CWD) in Colorado and Saskatchewan, Canada
- 04/24/2001 — Foot-and-Mouth Disease Spreads to Humans in England?
- 04/11/2001 — Foot-and-Mouth Disease – Why Slaughter?
- 03/26/2001 — Mad Cow and Foot and Mouth Disease Spreading
- 03/21/2001 — USDA Finally Removes 233 European Sheep from Vermont Farm After Court Battles
- 02/11/2001 — Update On Mad Cow Disease
- 01/21/2001 — Prions – The Misshapen Protein That Causes Mad Cow and CJ Disease
- 12/03/2000 — Bacteria from Outer Space?
- 09/24/2000 — Infectious Diseases – A Global Threat
- 11/15/1999 — Kunjin West Nile Fever Virus Update
- 10/12/1999 — Kunjin/West Nile Virus – First Time in Western Hemisphere
- 07/25/1999 — Maryland Fish Kills; Global Warming; and Warm Oceans and Disease
- 07/21/1999 — Warm Oceans and Disease: A Link
- 06/08/1999 — Increased Gray Whale Deaths in Spring 1999
- 05/30/1999 — Blowing Up Dangerous Germs with Oily “Nano Bombs”
- 05/27/1999 — Amphibian Decline – Parasites and Increased UV Radiation
- 05/10/1999 — New Bioterrorism Center
- 05/04/1999 — Mysterious Deaths of Harbor Porpoises on East Coast
- 02/07/1999 — Sulfur Bacteria, Whiskeytown, Calif.; Grackles, Louisiana
Websites:
E. coli O157:H7 Fact Sheet At CDC: http://www.cdc.gov/ncidod/dbmd/diseaseinfo/escherichiacoli_g.htm
Shigella: http://ohioline.osu.edu/hyg-fact/5000/5563.html
© 1998 - 2024 by Linda Moulton Howe.
All Rights Reserved.

